
You need to tell your ophthalmologist if you need to fly after having surgery. It also depends on whether you work and the type of work you do. The advice may be different depending on the type of surgery performed.

Your ophthalmologist will advise which activities should be avoided directly after the operation, and in the long term. Your vision may be blurry for a number of days, possibly weeks, following the surgery.

Eye drops will be given to help prevent infection and to control swelling. There may be some bruising and the eyelids may be sticky.
Vision loss, low vision and legal blindnessĪfter surgery, the eye will feel uncomfortable, possibly for a few weeks. Understanding the eye health profession. Posterior vitreous detachment (PVD) and floaters. Vitelliform macular dystrophy and Best disease. Reducing the risk of diabetic retinopathy. Detecting & monitoring changes in vision. The retinal surgeons at the Byers Eye Institute at Stanford are dedicated to restoring and preserving your sight and have access to the most advanced technologies and techniques available to repair your detached retina. This is generally appropriate for small detachments. Laser surgery-In certain cases, a retinal detachment can be walled off with laser to prevent the retinal detachment from spreading. The tear itself is sealed either with a freezing treatment at the time of the procedure, or with laser after the retina is re-attached. Pneumatic retinopexy-In this office-based procedure, a gas bubble is injected into the eye and the patient maintains a specific head posture to position the gas bubble over the retinal tear. The eye is then filled with a gas or oil bubble to hold the retina in place while it heals. A laser is used to seal the retinal tears or holes. Vitrectomy-Three small incisions (about 0.5 mm in size) are made in the white part of the eye and fine instruments are manipulated in the eye using an operating microscope to remove the vitreous gel that fills the eye and drain the fluid from under the retina. The fluid under the retina is sometimes removed at the time of surgery. The tear is treated with a freezing treatment to induce controlled scarring around the tear and permanently seal it. Scleral buckle-A silicone band is placed outside the eye to push the wall of the eye toward the retinal tear to close it. 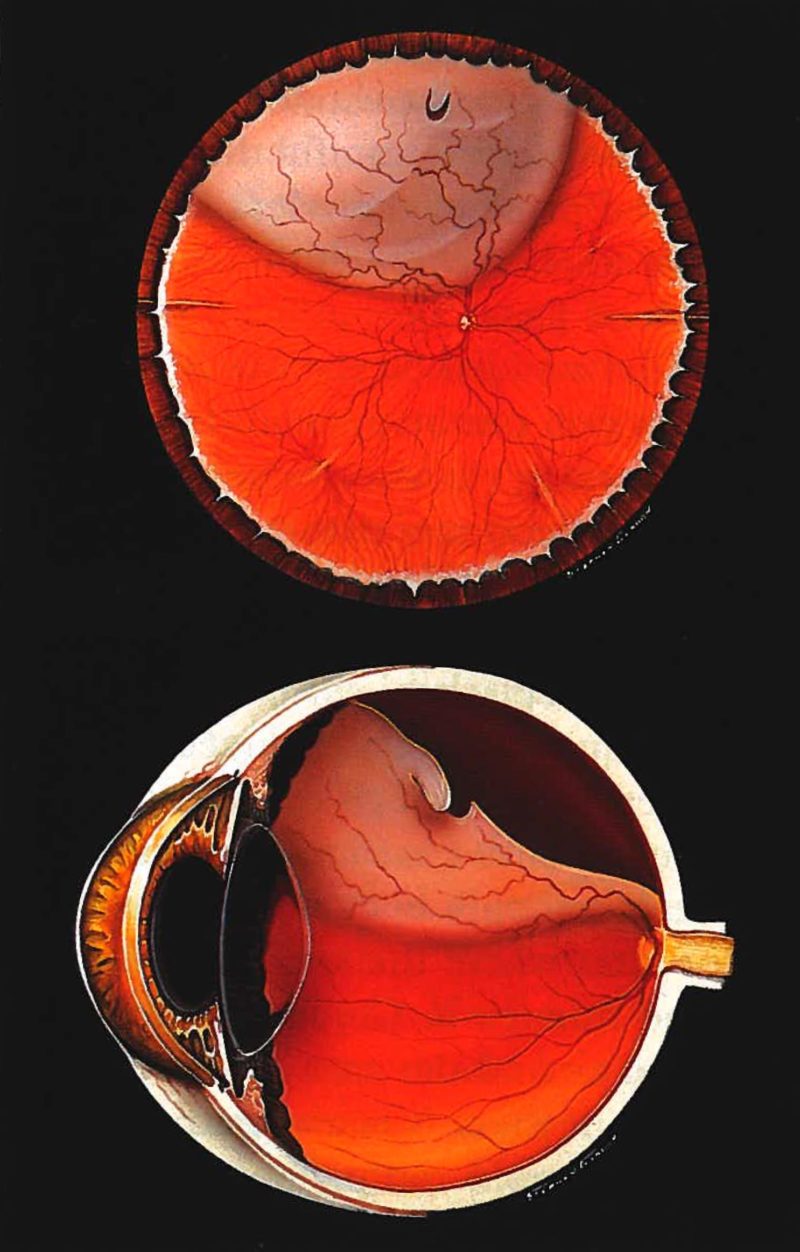
In general, retinal detachment repairs succeed about 9 out of 10 times, though sometimes more than one procedure is required to successfully re-attach the retina. Based on the characteristics of the detachment, your retinal surgeon can determine which approach is the most appropriate. Several approaches can be employed to repair a retinal detachment. The goal of treatment is to re-attach the retina to the back of the eye and seal the tears or holes that caused the retinal detachment.
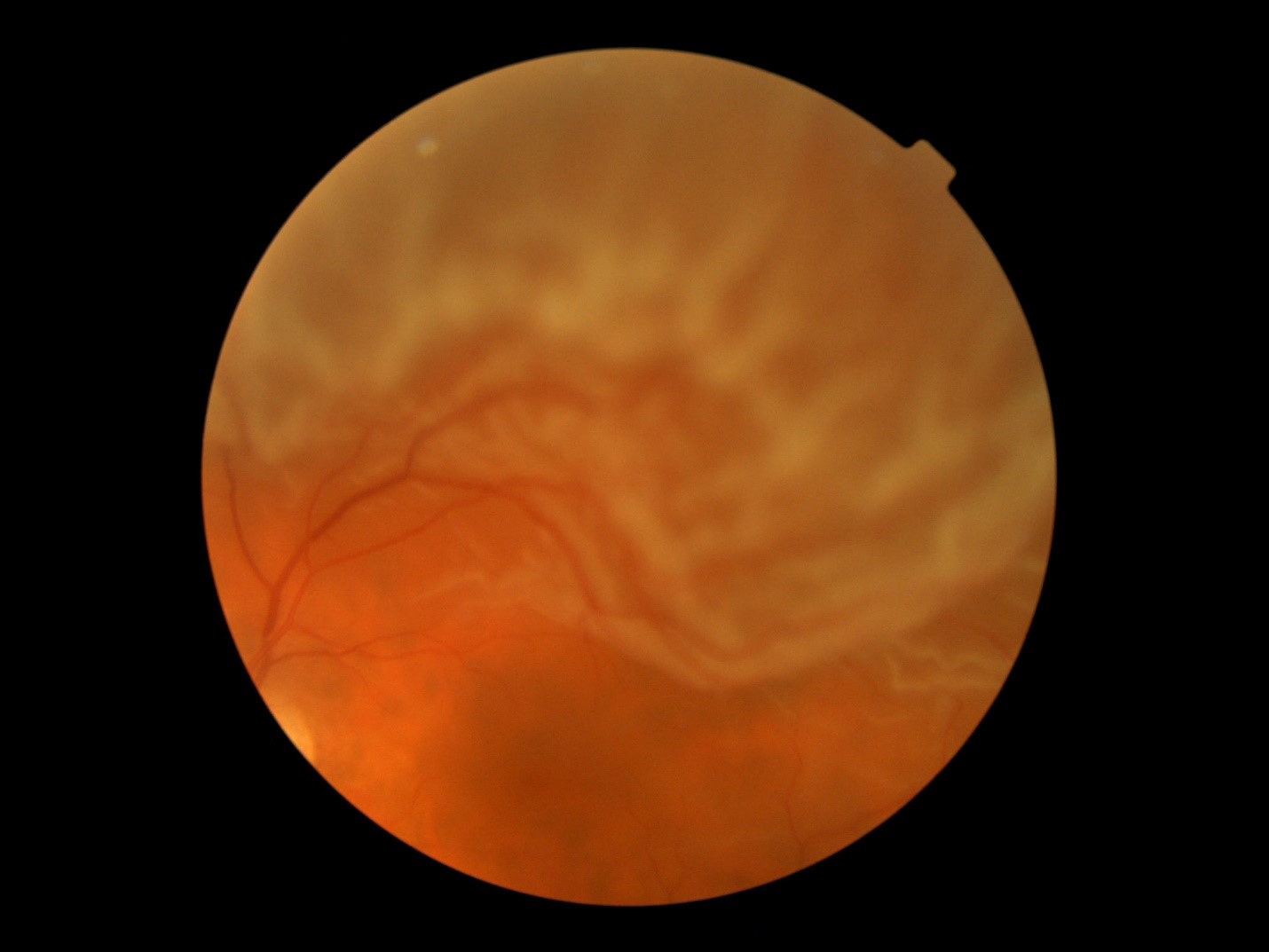
Lattice degeneration (thinning in the peripheral retina, or the area outside of the central retina.). Previous eye surgery, such as cataract surgery. Family history of retinal tears or retinal detachment. Risk factors for developing a retinal detachment include The typical symptoms of a retinal detachment include floaters, flashing lights, and a shadow or curtain in the peripheral (noncentral) vision that can be stationary (non-moving) or progress toward, and involve, the center of vision. When the retina is detached, it is separated from its blood supply and no longer functions properly. 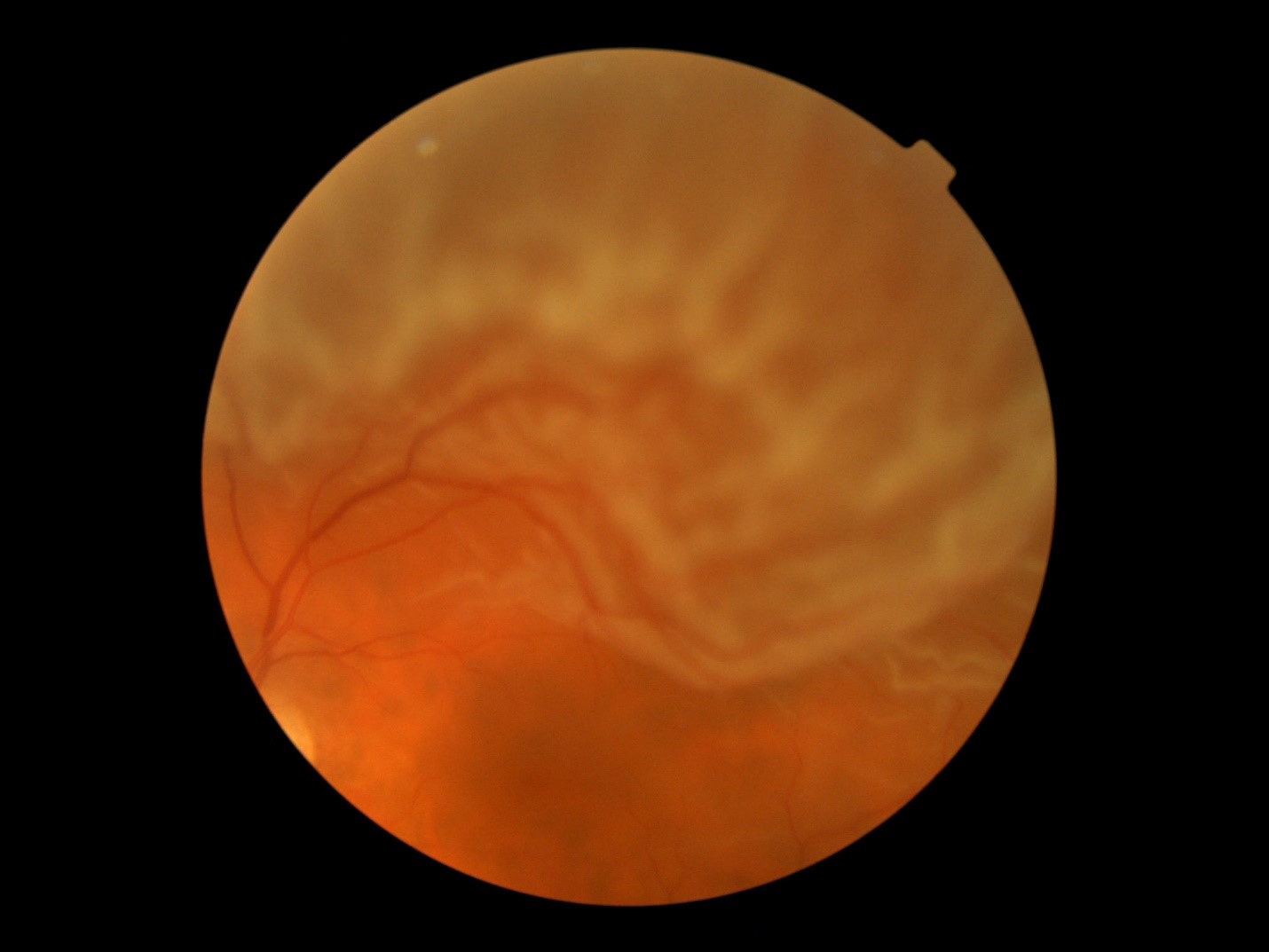
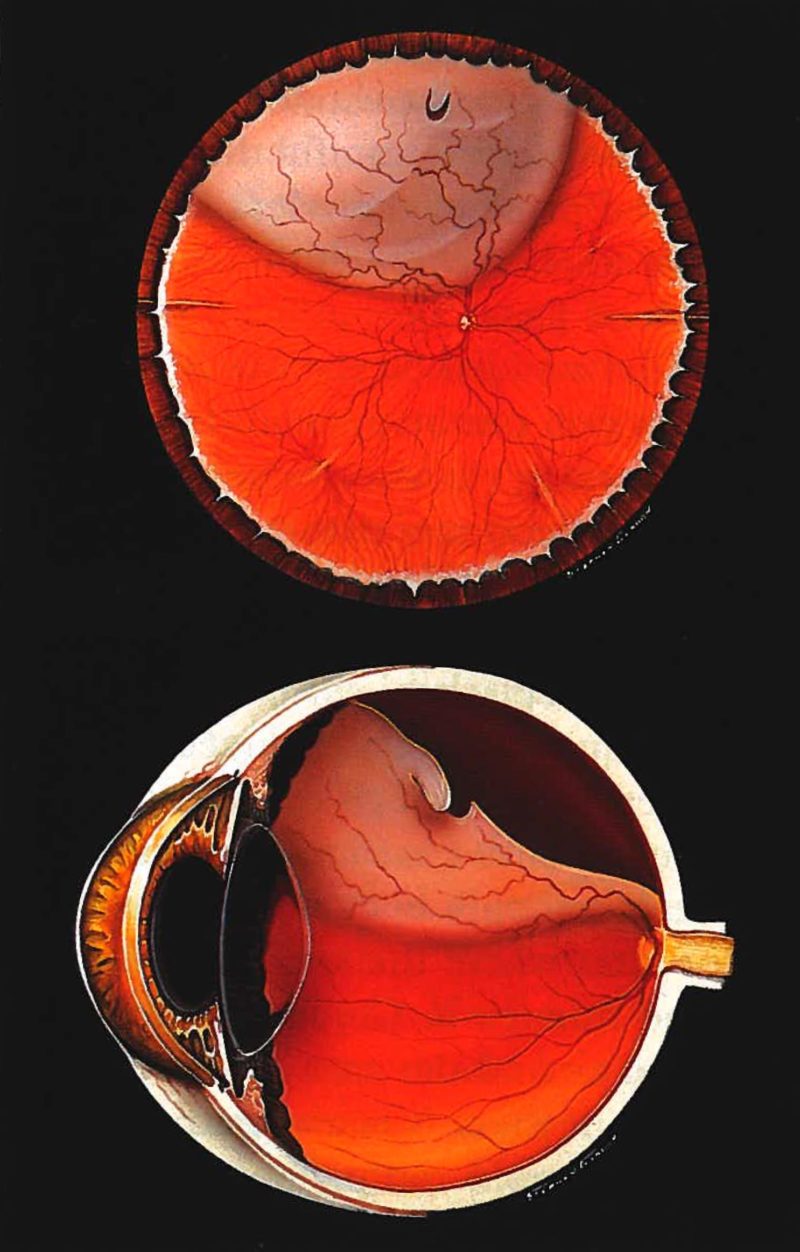
A retinal detachment occurs when the nerve tissue that lines the inside of the eye separates from the back wall of the eye, like wallpaper peeling off a wall. When the retina is detached, it is separated from its blood supply and no longer functions properly.






 0 kommentar(er)
0 kommentar(er)
